Chronic wounds are more than just a physical ailment; they often carry a significant emotional and financial burden for those affected.
These wounds can persist for weeks or even months, resisting conventional treatments and posing serious health risks.
In Singapore, advanced medical interventions provided by experienced specialists can help manage and heal chronic wounds effectively.
This guide explores everything you need to know about chronic wound treatment in Singapore, from understanding the causes and risks to a comprehensive suite of treatment options and preventive strategies.
Understanding Chronic Wounds (or Non-Healing Wounds)
What Are Chronic Wounds?
Wounds that do not heal after an extended period, about three months, are generally considered chronic. In many cases, these wounds may take years to heal or might never fully close without proper medical intervention.
Factors that can impact wound healing include underlying conditions such as diabetes, venous or arterial diseases, infections, and age-related metabolic deficiencies.
Symptoms and Types of Chronic Wounds
Chronic wounds can vary in their causes and characteristics, but they all share the common trait of delayed healing. Below are the most common types of chronic wounds, along with their unique features and challenges:
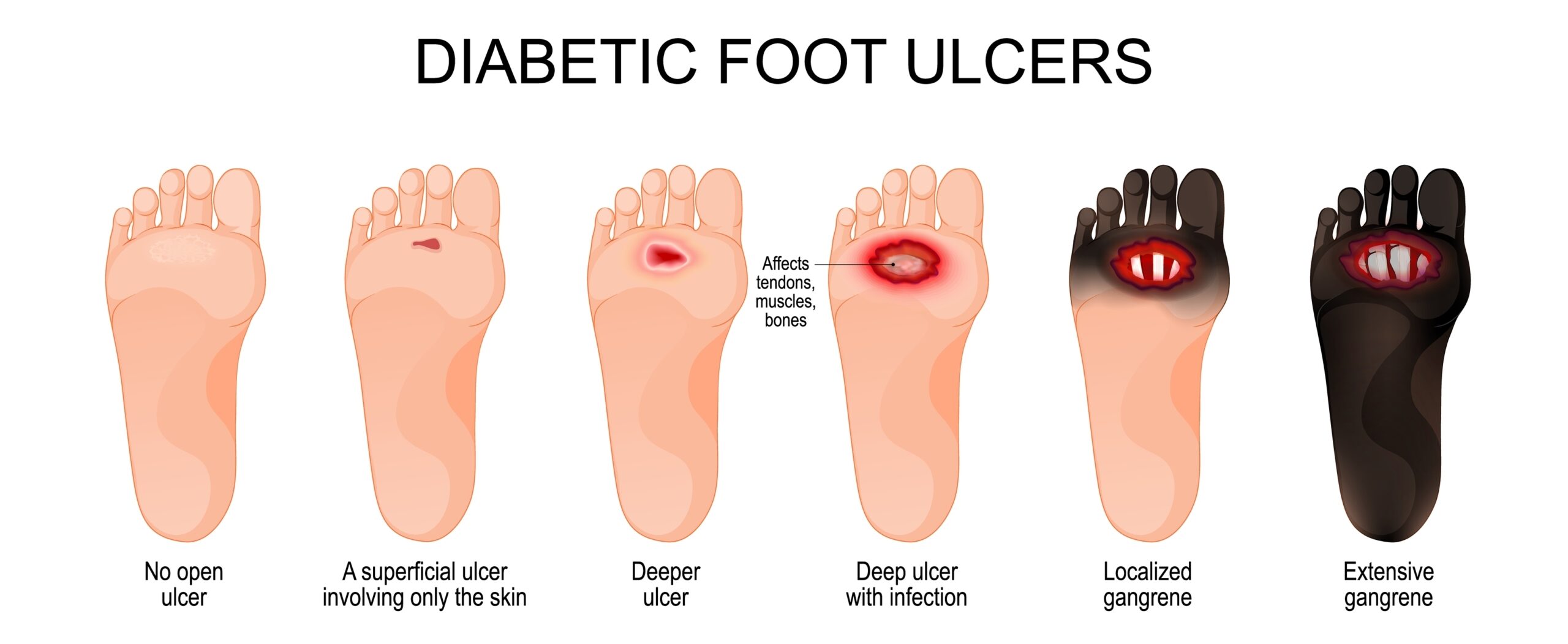
1. Diabetic Foot Ulcers
Diabetic foot ulcers are one of the most prevalent types of chronic wounds, particularly among individuals with poorly managed diabetes. They typically develop on the feet and are caused by a combination of factors:
- Nerve Damage (Neuropathy): Reduces sensation, making it easier to sustain unnoticed injuries.
- Poor Circulation (Peripheral Artery Disease): Impairs blood flow to the lower extremities, slowing tissue repair.
- Infection Susceptibility: High blood sugar levels can weaken the immune system, making these wounds prone to infection.
Without proper treatment, diabetic foot ulcers can lead to severe complications, including infection and, in extreme cases, amputation.
2. Venous Leg Ulcers
Venous leg ulcers occur when veins in the lower legs fail to return blood efficiently to the heart, causing blood to pool in the veins. This increased pressure can damage the surrounding skin and tissues, resulting in open sores, typically on the inner part of the lower leg.
Key characteristics include:
- Swelling (Edema): Often accompanied by achy, swollen legs.
- Discoloration: Skin around the ulcer may appear darkened or hardened.
- Recurring Nature: These ulcers are prone to reappearing even after treatment.
Proper compression therapy and addressing the underlying venous insufficiency are critical to managing venous ulcers.
3. Arterial Ulcers
Arterial ulcers, also known as ischemic ulcers, develop when blood flow to the tissues is restricted due to narrowed or blocked arteries. Commonly found on the feet, toes, or other areas with poor circulation, these ulcers can present with:
- Sharp Pain: Often worsened when the legs are elevated.
- Cool, Pale Skin: Surrounding the ulcer due to lack of blood supply.
- Well-Defined Edges: The ulcers are usually small and have a punched-out appearance.
Arterial ulcers require urgent medical attention to restore blood flow and promote healing.
4. Pressure Ulcers
Pressure ulcers, also known as bedsores, form when prolonged pressure on the skin reduces blood flow, typically affecting individuals with limited mobility.
Common sites include bony areas such as the tailbone, hips, heels, and elbows. Key features include:
- Stages of Severity: Ranging from redness in the skin to deep wounds exposing bone or muscle.
- High Risk in Bedridden Patients: Often seen in those confined to beds or wheelchairs.
- Preventable: Regular repositioning and specialized mattresses can help reduce the risk.
5. Traumatic or Surgical Wounds
Wounds resulting from surgery or injury can become chronic if healing is disrupted. Factors like infections, poor wound care, or underlying conditions such as diabetes can delay recovery.
These wounds often require additional interventions to prompt the healing process.
6. Chronic Infected Wounds
Some chronic wounds, regardless of their origin, become persistently infected. Infected wounds often show:
- Signs of Infection: Redness, swelling, warmth, or foul-smelling discharge.
- Delayed Healing: As the immune response is focused on fighting the infection rather than repairing tissue.
- Potential Systemic Effects: Severe infections can spread, causing complications such as cellulitis or sepsis.
Who is at Risk?
Certain individuals are more prone to developing chronic wounds due to underlying health issues or lifestyle factors. These include:
- People with Diabetes – Poor circulation and nerve damage increase the risk of non-healing wounds, especially diabetic foot ulcers.
- Those with Poor Circulation – Conditions like peripheral artery disease or venous insufficiency impair blood flow needed for healing.
- Elderly Individuals – Slower healing processes and thinner skin make older adults more vulnerable.
- Bedridden or Immobile Patients – Prolonged pressure on the skin can cause pressure ulcers.
- Smokers – Reduced blood flow and oxygen delivery hinder wound recovery.
- Individuals with Chronic Illnesses – Conditions like heart disease, kidney disease, or autoimmune disorders delay healing.
- Obese Individuals – Excess weight adds pressure to the skin and affects circulation.
If you or someone you know is at higher risk, early intervention and proper care are crucial to prevent complications.
Why Prompt Treatment is Crucial

Preventing Severe Complications
Prompt treatment of chronic wounds is essential to avoid severe complications that can significantly impact your health and quality of life.
When left untreated, chronic wounds can lead to severe pain, tissue damage, and infections that may spread to the bloodstream — known as sepsis, a potentially life-threatening condition.
For individuals with diabetes, the risk is even greater, as infections can progress rapidly and result in complications that may require amputation. Delayed treatment can also lead to chronic pain and deep tissue damage, making recovery more difficult.
Early intervention addresses not only the wound but also underlying issues like poor circulation or diabetes, reducing the risk of serious outcomes.
Chronic Wounds: A Healthcare Challenge
Chronic wounds represent a significant healthcare challenge due to the underlying conditions that often go unrecognised:
Many patients view wounds as isolated issues and may not realize that they could be signs of deeper problems, such as vascular disorders, diabetes, or other systemic health concerns.
This lack of awareness often delays seeking appropriate medical care, allowing the wound to worsen and the underlying condition to remain untreated.
For example, a wound that fails to heal may be a result of poor blood circulation caused by a vascular disorder:
However, without understanding this connection, patients might focus solely on treating the wound’s surface, using over-the-counter remedies or basic first aid. These approaches, while helpful for minor injuries, are insufficient for chronic wounds and do not address the root cause.
Notice a wound that’s slow to heal? Schedule a consultation with our wound care specialists today.
Diagnosing Chronic Wounds

Diagnosing chronic wounds involves more than just examining the wound itself — it requires identifying the underlying causes that may delay healing. A thorough assessment ensures the right treatment approach.
1. Medical History and Physical Examination
- Your doctor may begin by reviewing your health history and examining the wound’s size, depth, and signs of infection. Conditions like diabetes or poor circulation are also considered.
2. Imaging Tests
- Tests like Doppler ultrasound assess blood flow, while X-rays or MRIs check for deeper infections or bone involvement.
3. Laboratory Tests
- Wound Cultures: Identify infections and determine suitable antibiotics.
- Blood Tests: Reveal issues like high blood sugar or systemic infections.
4. Specialised Tests
- Additional tests, such as the Ankle-Brachial Index for circulation issues or venous ultrasound for vein function, may pinpoint the root cause of delayed healing.
Treatment for Chronic Wounds

Treating chronic wounds requires a comprehensive approach tailored to the wound’s cause, severity, and the patient’s overall health.
Treatment often involves addressing the wound itself while managing any underlying conditions that may hinder healing.
Depending on the case, non-surgical or surgical options may be recommended:
Non-Surgical or Minimally-Invasive Approaches
Non-surgical treatments focus on creating the optimal environment for wound healing while addressing the root cause of delayed recovery. These approaches include:
1. Advanced Wound Dressings
- Specialised dressings like foam, hydrocolloid, or alginate maintain moisture, protect against infection, and promote healing.
2. Wound Debridement
- Removing dead or infected tissue allows healthy tissue to regenerate and improves the effectiveness of other treatments.
3. Compression Therapy
Essential for venous ulcers, compression bandages or stockings improve blood flow and reduce swelling.
4. Negative Pressure Wound Therapy (NPWT)
- Also known as vacuum-assisted therapy, NPWT removes excess fluid and stimulates tissue growth by applying controlled suction to the wound.
5. Topical or Hyperbaric Oxygen Therapy (HBOT)
- Hyperbaric Oxygen Therapy (HBOT) involves delivering oxygen in a pressurized chamber, significantly increasing oxygen levels in the wound to accelerate healing, particularly in cases like diabetic foot ulcers.
6. Medications and Infection Control
- Antibiotics are prescribed to treat infections, while medications may be recommended to manage underlying conditions such as diabetes or circulatory disorders.

Surgical Interventions
When non-surgical approaches are insufficient, surgical treatments may be necessary to repair tissue, address circulation problems, or close the wound. These include:
1. Split Skin Grafting
Skin grafting is a procedure which involves removing the top layer of skin from one area of the body, usually the thigh, and moving it to cover large wound defects.
Over the next few days, tiny blood vessels grow into the graft, establishing a blood supply that helps it integrate with the surrounding tissue
Skin grafting has been shown to increase the healing rate of diabetic foot ulcers and minimise complications which may require major lower limb amputation.
2. Vascular Surgery
Vascular surgery plays a vital role in treating chronic wounds by enhancing blood flow to the affected area, a critical factor for healing.
Procedures such as angioplasty, stenting, and bypass surgery restore arterial circulation (i.e., blood inflow to the wound), while vein treatments improve venous blood flow (i.e., blood outflow).
Both are essential to creating the conditions needed for optimal wound healing.
By addressing circulation issues, vascular surgery not only facilitates wound repair but also supports other treatments like advanced dressings or skin grafts and lowers the risk of recurring wounds:
This approach is especially important for patients with conditions like peripheral artery disease or chronic venous insufficiency.
Whenever possible, keyhole techniques are used, allowing for smaller incisions that minimise trauma and promote a faster, smoother recovery.
Don’t let chronic wounds weigh you down further. Consult our specialist for an evaluation today.
Cost of Chronic Wound Treatment in Singapore

A comprehensive chronic wound treatment plan includes specialised diagnosis, procedures, and aftercare. Below are the cost ranges for various procedures, with surgical fees adhering to the Ministry of Health (MOH) benchmarks:
Note: The costs listed below reflect only the surgeon’s fees and exclude VAT, in-clinic consultations, hospital charges, and other consumables. The final bill may vary depending on the procedures recommended and the complexity of each case.
Procedures with assigned surgical codes may qualify for subsidies through insurance or Medisave. Additionally, fees for doctor consultations and aftercare may be claimable for treatments associated with a surgical code.
Diagnosis Cost Ranges (SGD)
CT Scan
$1,000 – $1,500
MRI with Contrast
$1,500 – $3,000
Duplex Ultrasound (Unilaterel)
$500 – $1,000
Chronic Wound Procedures Cost Ranges (SGD)
Wound Debridement
Code: SA811S
$1,600 – $3,600
Wound Debridement, Repair of Multiple or Deeper Wounds
Code: SA842S
$3,600 – $5,600
Split Skin Grafting
Codes: SA822S to SA826S
$750 – $10,200
Vascular Procedures Cost Ranges (SGD)
Artery, Percutaneous Angioplasty (PTA)
Code: SD720A
$6,700 – $11,200
Vein, Percutaneous Angioplasty (PTA)
Code: SD710V
$2,800 – $5,600
Diagnostic Angiogram
Codes: SD725A
$2,100 – $3,600
Diagnostic Venography
Code: SD706V
$1,100 – $2,500
Insurance and Medisave Coverage
Chronic wound treatment modalities with an assigned surgical code may qualify for subsidies under insurance health plans or Medisave. The claimable amount depends on the procedure and the guidelines set by the Ministry of Health (MOH).
We encourage you to contact our clinic to consult our doctors about the treatment plan best suited to your condition and discuss your financing options.
Preventing Chronic Wounds and Enhancing Recovery

Managing chronic wounds goes beyond treatment—it involves making long-term changes to prevent recurrence and support the healing process.
With the right lifestyle modifications and wound care strategies, you can significantly improve your recovery and maintain better overall health.
Lifestyle Modifications for Better Wound Healing
- Eat a Balanced Diet: Include lean proteins, fruits, and vegetables to boost tissue repair.
- Quit Smoking: Smoking reduces circulation and delays healing.
- Stay Active: Light exercises, like walking, improves blood flow.
- Manage Chronic Conditions: Keep diabetes or hypertension under control to reduce risks.
- Maintain a Healthy Weight: Lower body strain helps wounds heal better.
Long-Term Wound Care Tips
- Keep the Wound Clean: Follow medical advice for cleaning and dressing your wound.
- Monitor for Infection: Look for redness, swelling, or discharge, and consult a doctor if needed.
- Post-Treatment Instructions: Stick to your prescribed treatment plan and attend follow-ups.
- Avoid Trauma: Protect the wound area from pressure or injury.
- Stay Hydrated: Good hydration supports tissue healing.
Frequently Asked Questions (FAQ)
What are chronic wounds, and how do they differ from regular wounds?
Chronic wounds are injuries to the skin or underlying tissue that fail to heal within three months.
Unlike regular wounds, which heal naturally within weeks, chronic wounds often result from underlying conditions like diabetes, poor circulation, or infections, requiring specialized care.
What are the signs that a wound has become chronic?
A wound may be chronic if it shows no signs of healing after several weeks, worsens over time, or exhibits symptoms like redness, swelling, warmth, foul-smelling discharge, or persistent pain.
If you notice any of these signs, consult a specialist for a medical evaluation.
Can chronic wounds heal on their own?
Most chronic wounds won’t heal without medical intervention. Treating the wound and addressing underlying causes, such as poor circulation or infections, is essential to promote healing and prevent complications.
What treatments are available for chronic wounds?
Treatment options include advanced dressings, wound debridement, compression therapy, hyperbaric oxygen therapy, and, in severe cases, surgical interventions like skin grafting or vascular surgery. The best treatment depends on the wound’s cause and severity.
What to Expect During the Treatment Process?
- Initial Consultation and Assessment: Your first visit involves a detailed evaluation of the wound’s size, depth, and condition. Diagnostic tests may also be performed to identify underlying issues.
- Creating a Personalised Treatment Plan: Every wound is unique, and so is the treatment. Our specialists consider factors like wound type, patient health, and risk factors to develop an individualised care plan.
- Ongoing Monitoring and Adjustments: Regular follow-ups are essential to monitor progress and modify the treatment plan if necessary, ensuring optimal healing outcomes.
Chronic Wound Care at The Vascular and Endovascular Clinic

At The Vascular and Endovascular Clinic, we take a personalized approach to care, utilizing evidence-based procedures to ensure safe and optimal outcomes for our patients.
Our practice is led by experienced vascular and wound care specialists, Dr. Julian Wong and Dr. Tang Tjun Yip. Dr. Tang is an accredited Certified Wound Specialist Physician by the American Board of Wound Management (ABWM), highlighting his expertise in wound care.
With over 20 years of experience and more than 300 peer-reviewed publications, patients can expect to be in good hands under the care of our specialists.
References:
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7520842
Incidence of Chronic Wounds in Singapore: This study examines the one-year incidence rates of chronic wounds among patients in various hospital settings in Singapore, reporting rates ranging from 11% to 18%. - https://bmjopen.bmj.com/content/13/9/e065692
Economic Burden of Chronic Wounds: Research published in BMJ Open highlights the significant healthcare costs associated with chronic wounds in Singapore and suggests that investments in comprehensive wound prevention and treatment programs can reduce these costs. - https://www.duke-nus.edu.sg/newshub/media-coverage/chronic-wounds-significant-health-and-economic-burden
Singapore Wound Registry: The Singapore Wound Registry serves as a platform for assessing the national wound burden, gathering data on wound outcomes, tracking management costs, and evaluating the impact on quality of life. - https://journals.cambridgemedia.com.au/wpr/volume-24-no-3/economic-evaluation-chronic-wound-management-tertiary-hospital
Economic Evaluation of Chronic Wound Management: A study conducted at Singapore General Hospital provides an overview of the direct and indirect costs of managing chronic wounds, offering a reference for future interventions. - https://onlinelibrary.wiley.com/doi/10.1111/iwj.13708
Health-Related Quality of Life and Chronic Wound Characteristics: This research explores the increased prevalence of chronic wounds in Singapore and the associated clinical and economic burdens related to extended wound care.
Disclaimer: The information and content provided in this guide are for informational purposes only. They are not intended to replace professional medical consultation, diagnosis, or treatment, nor to endorse any particular treatment option.