Quality of life impacted by non-healing wounds? Seek treatment from our Vascular Specialists.
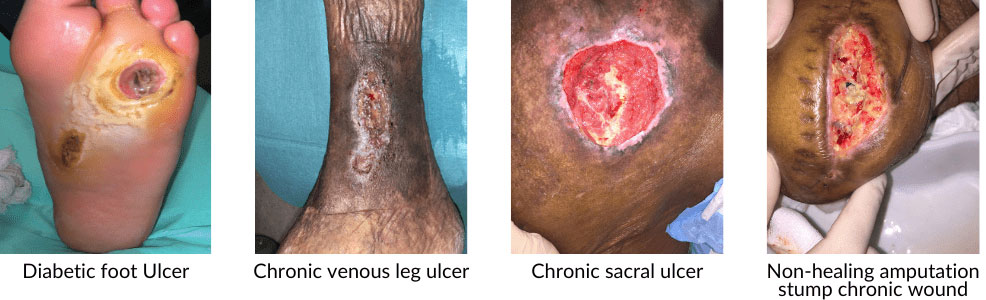
What are Chronic Wounds?
Chronic wounds are wounds that do not heal in an orderly and timely manner, as most acute wounds would. Wounds that do not heal over a long time (about 3 months), are often considered as chronic.
Chronic wounds can cause patients severe emotional and physical stress and create a significant financial burden over the long term.
Our clinic provides comprehensive, up-to-date and evidence-based wound healing management therapies. Dr. Tang Tjun Yip has been previously certified by the American Board of Wound Management (ABWM).
Your hard to heal wound will be evaluated carefully and a customised individual treatment plan will be developed to optimise wound healing trajectory for you.